DiaLog
A patient centered service to navigate diagnosis uncertainties by symptom tracking, sense making, and consultation preparation.
-
As part of the Philips Student Service Design Challenge: Expanding Self-Confidence Horizons, this project explored how self-care can support emotional resilience and confidencenot just physical health.
Through our research, we identified diagnosis limbo as a critical but underserved self-care gap for women aged 25–45 in the UK. During prolonged periods of medical uncertainty, patients are expected to manage symptoms, emotions, and decisions independently and often without validation, continuity, or support.
-
This project was delivered by Richa Kejriwal, Maya Burnand, Miran Jurisevic, Lucia Perez Gonzalez, Kate Winbaum, Jessica Wonomihardjo and Vivien Fergusson.
Owned research operations and strategic synthesis: recruiting participants, designing and conducting qualitative research with patients and healthcare providers, facilitating workshops, and shaping the service strategy and concept direction -
DiaLog is a patient-centred digital service designed to support women navigating diagnosis limbo before, during, and between clinical touchpoints.
THE CHALLENGE
An estimated 5.7 million women in the UK are awaiting diagnosis. The average women’s health diagnostic journey is 2 years 3 months, and conditions like endometriosis can take up to 8 years. But the problem isn’t only time. The experience becomes harmful when care is:
Fragmented (patients lose continuity and repeat their story)
Compressed (many GP consultations last 15–20 minutes)
Emotionally unsafe (patients report dismissal, “gaslighting,” or unpredictability across clinicians)
Information misunderstood (self-diagnosis and misinformation can amplify anxiety)
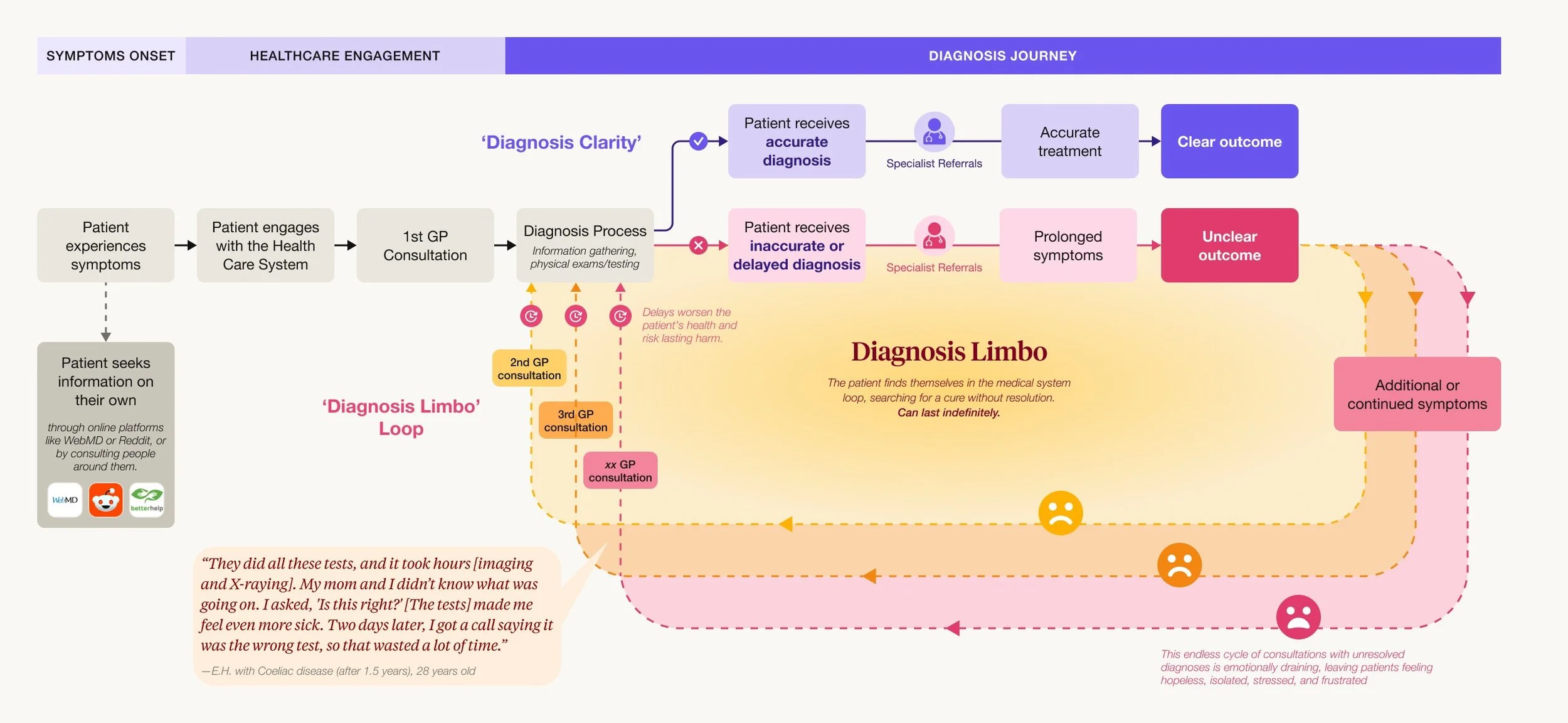
Image: Patient Journey Map
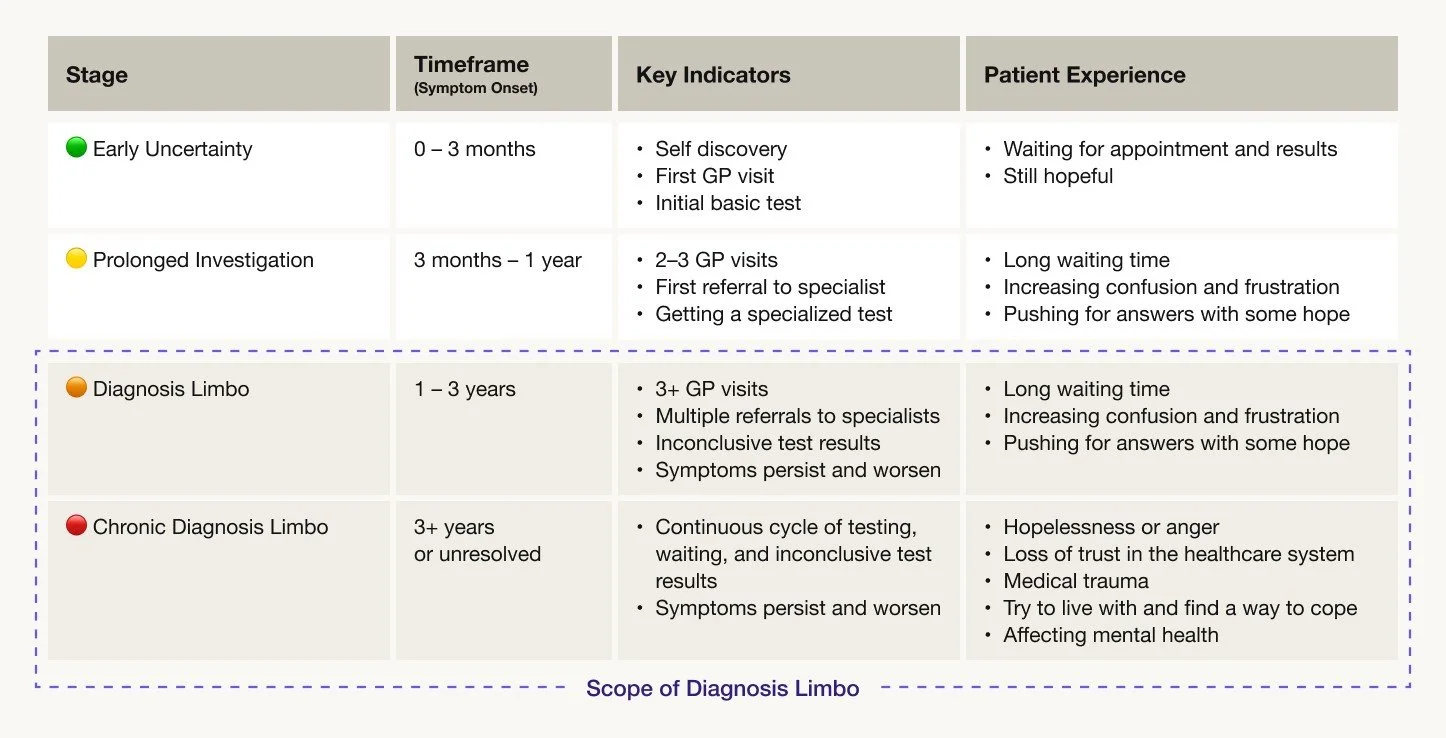
Diagnosis Limbo is a prolonged period of uncertainty
when someone has symptoms but no clear diagnosis
Image: Stages of Diagnostic Limbo
RESEARCH INSIGHTS
20 IN DEPTH INTERVIEWS (13 PATIENTS & 7 HEALTHCARE PRACTITIONERS)
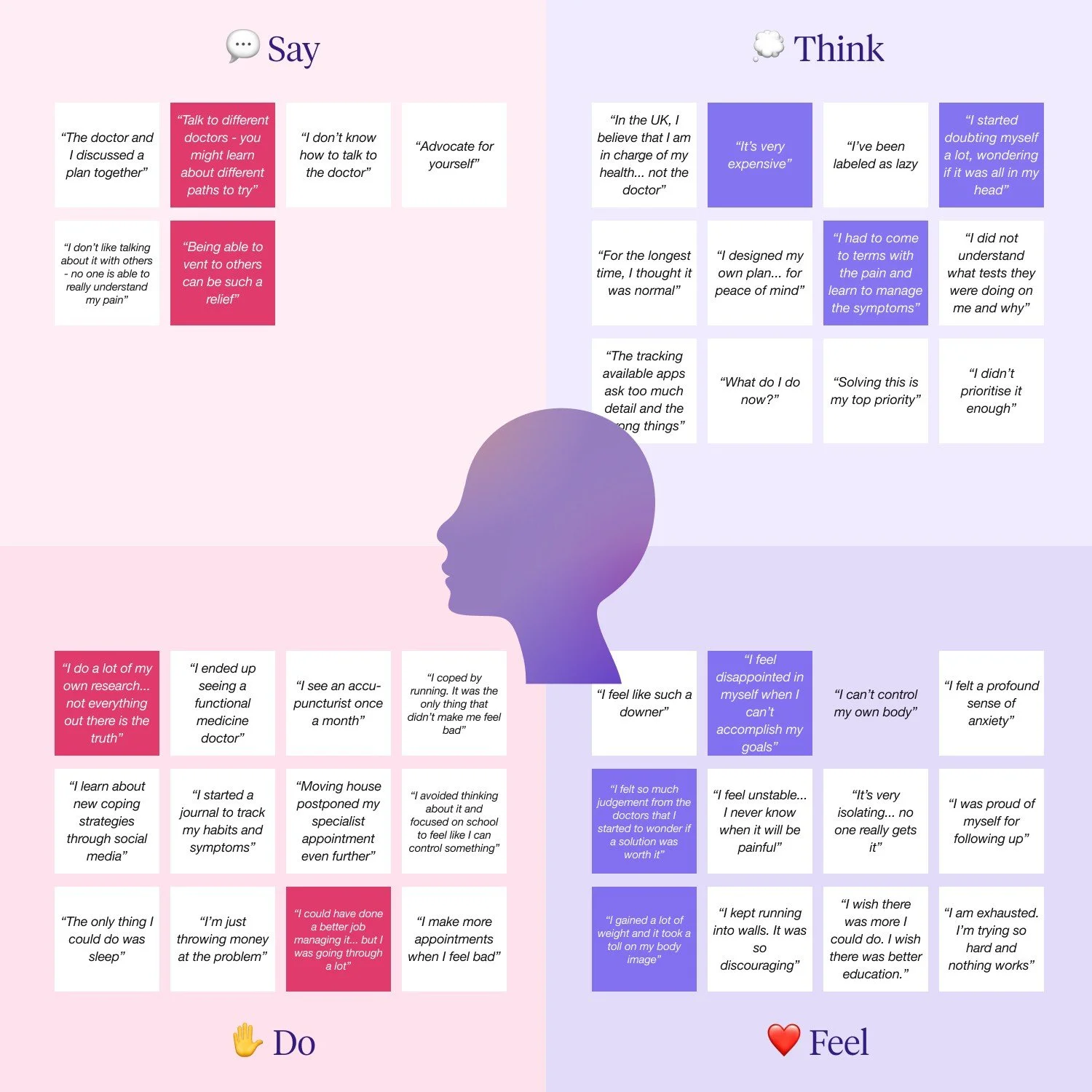
Image: Patient empathy map based on patient audio/ video interviews.
PATIENT’S CHALLENGES
Patients feel marginalised and alone
Despite how common this experience is, every interviewee described feeling isolated in their journey — especially when their condition lacked a clear name or diagnosis.
Communication is frustrating
Patients often feel dismissed or gaslit by medical professionals, while also struggling to piece together or recall patterns in their own symptoms and experiences.
Failed by the healthcare system
Systemic failures make the journey feel endless and disheartening. Many patients expressed a desire to regain control, often resorting to self-advocacy and independent research to find answers.
HEALTHCARE PRACTITIONER’S (HCP) CHALLENGES
HCPs must run a tight schedule
Most GP visits last 15–20 minutes, with HCPs juggling patient care and admin. There is a high demand for appointments, but a limited capacity to deliver them, leading to rushed consultations and patient dissatisfaction.
Rise of self-diagnosis
Patients often turn to the internet for answers. While it can empower them, it also risks misinformation and anxiety, sometimes complicating appointments or delaying proper treatment.
HCPs may react to patients’ emotions in differently
Patients often arrive feeling emotional or frustrated. Some HCPs may take this personally, while others feel sympathy and try to offer extra support. Since patients rarely see the same doctor, reactions vary, making the doctor-patient relationship feel unpredictable.
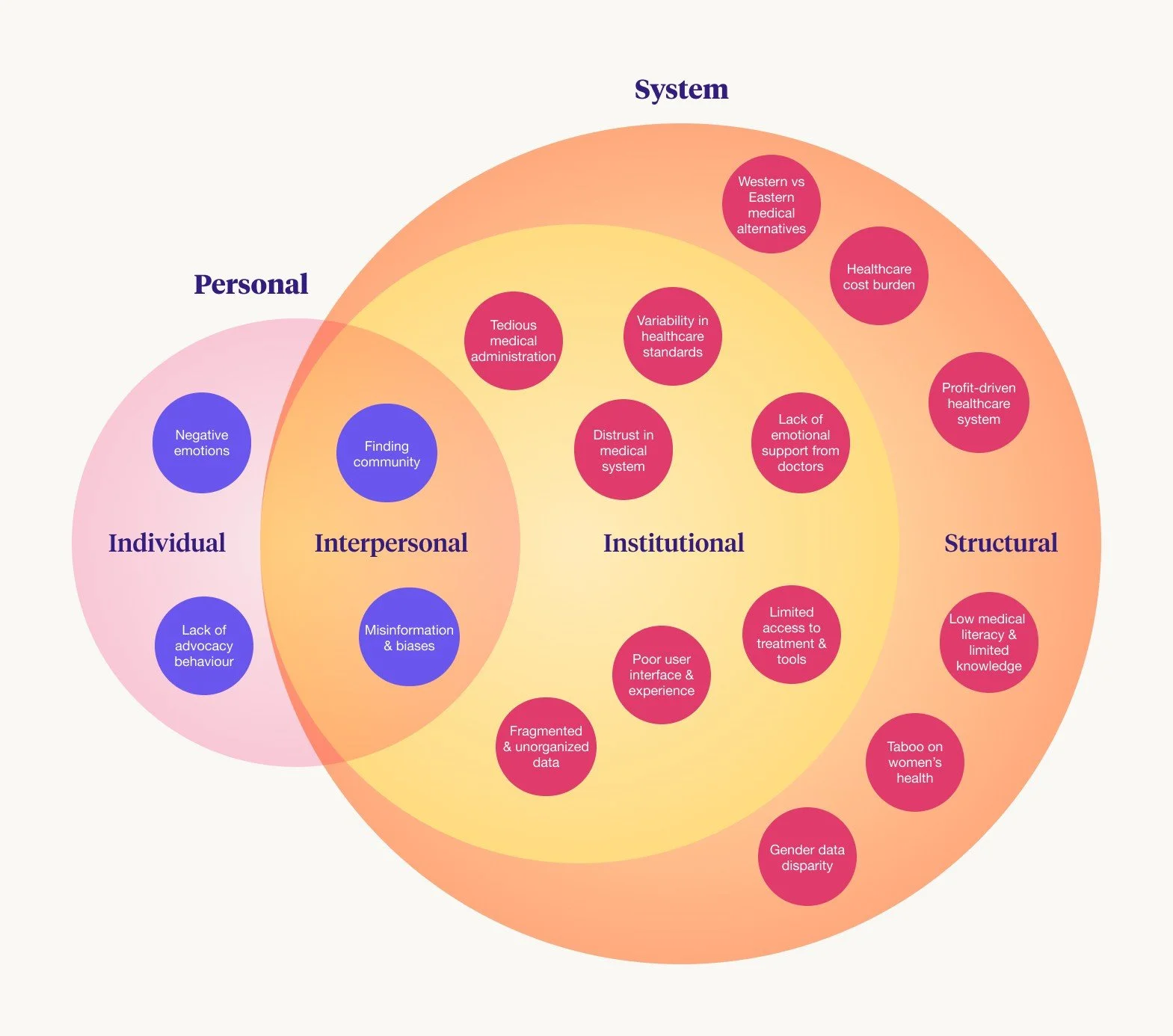
Image: Problem Mapping categorised, synthesised and organised based on the scale of control.
INDIVIDUAL & INTERPERSONAL LEVEL CHALLENGES
Advocacy Behaviour
Patient advocacy varies based on how individuals navigate diagnosis limbo.
Negative Emotions
Patients in diagnosis limbo often face overwhelming negative emotions.
Community & Biases
Many patients in diagnosis limbo feel isolated as they struggle to find relatable supports. .
INSTITUTIONAL & STRUCTURAL LEVEL CHALLENGES
Medical Administration
Long wait times and difficulty booking appointments make navigating the system stressful.
Doctor-Patient Relationship
Doctors often fail to provide emotional support due to the lack of a personal relationship.
Fragmented Data & Poor UX
Fragmented medical data forces patients to repeatedly explain their history to different doctors.
Healthcare Cost Burden
Diagnosis limbo burdens the healthcare system, with delays leading to inefficiencies and economic losses.
Medical Literacy & Education
Many struggle to navigate medical information that is complex and often inaccessible.
Gender Inequality in Healthcare
Women’s health is stigmatized in society and under researched leading to gender data gap in the system.
DESIGN OPPORTUNITY
How might we empower women in the UK who are experiencing the challenges of Diagnosis Limbo to feel supported through their journey so they can receive the care they deserve?
REFRAME & REDEFINE
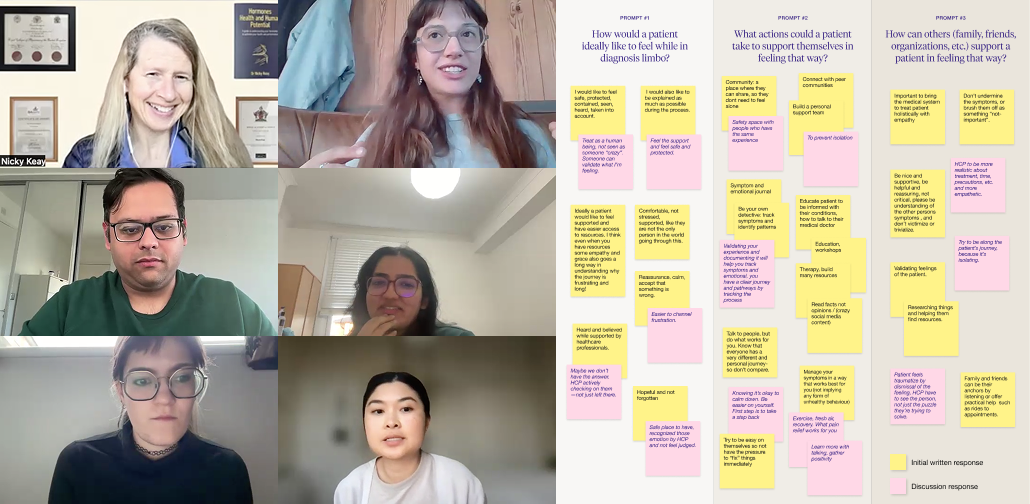
Image: Co-design workshop, engaging both patients, medical practitioners.
Interviews and co-design workshops have deepened our understanding of both patient and healthcare provider behaviours. Initial ideation spanned across experiential, technological, financial, and social models.
Self-initiated suggestions looked at behavioural change for the patient like tools to develop the skills necessary to be a more confident and informed self-advocate, and to manage emotional and mental wellbeing. Systems-led ideas mapped touchpoints in both the public and private sectors that could serve as leverage points to improve patient experiences and enhance interactions for both patients and providers.
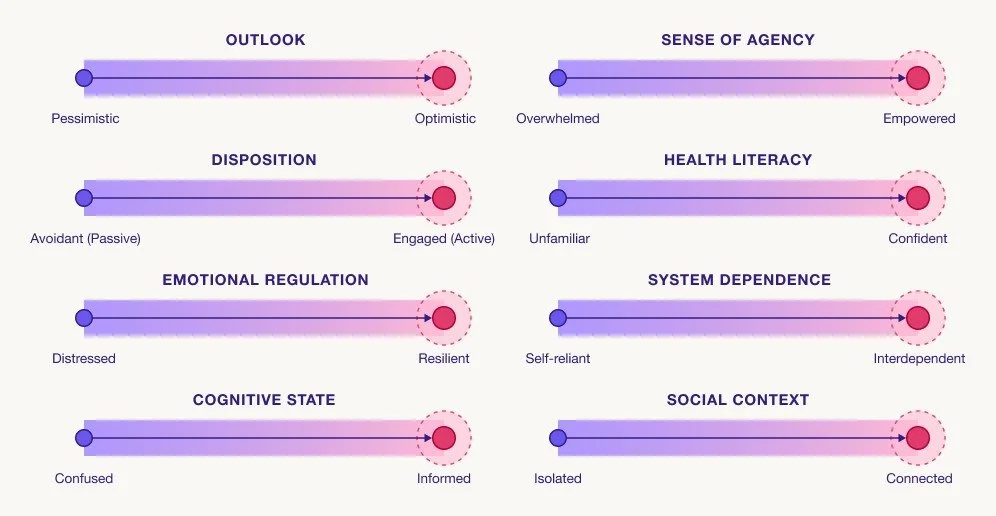
Image: Mapping patient behavioural traits
KEY TAKEAWAY
A patient’s mindset is a key factor in navigating the uncertainty of diagnosis limbo, especially when external systems fall short in providing support. Developing the right mindset can empower patients to take an active role in managing their health, even in the face of ambiguity. Factors such as outlook, disposition, emotional regulation, cognitive state, health literacy, sense of agency, system dependence, and social context all influence how patients cope with this challenging period.
BREAKTHROUGH
Diagnosis limbo should not be treated merely as the absence of a diagnosis rather a diagnosis in itself.
STRATEGY & SOLUTION
Introducing DiaLog, a platform-as-a-service, empowers patients to track symptoms, store records, and access trusted medical insights. It offers personalized guidance for medical conversations, connects users with global doctors, and visualizes key health patterns. Patients can find and connect with others on similar journeys and contribute to research that advances gender inclusive care.
Image: Patient facing App - DiaLog
Image: Screen from DiaLog App
PATIENT FACING APP FEATURES
-
DiaLog allows patients to track their symptoms flexibly through voice notes, photos, journal entries, or by scanning images. It consolidates medical records, symptom logs, doctor notes, appointment schedules, and personal reflections in one secure place, enabling both patients and healthcare providers to see the full picture and stay aligned, informed, and proactive.
-
Draws personalised, actionable insights from the patient’s health repository by cutting through the noise. Is based on patient and community input, using a smart information tagging system. It also visualises each patient’s medical journey, highlighting key trends and turning points to support better understanding and decision-making.
-
DiaLog provides guidance on navigating difficult medical conversations, from know-how tips, conversation prompts, and preparation guides. Empowering individuals to communicate effectively, ask the right questions, and advocate for themselves throughout their health journey.
With its built-in Chat AI feature, DiaLog helps users prepare for medical visits, ensuring more meaningful consultations and better communication of their health experiences.
-
DiaLog provides access to a library of vetted clinical studies, research papers, and educational materials tailored to your symptoms and health journey. It also connects patients to verified medical professionals worldwide through telemedicine, offering second opinions and diverse perspectives to help them stay informed, confident, and no longer limited by local healthcare boundaries.
-
DiaLog connects patients with others experiencing similar symptoms and journeys, fostering a sense of empowerment, validation, understanding, and being truly heard. It nurtures emotional connection by celebrating small milestones, tracking personal growth, and encouraging peer advocacy.
DIALOG: SERVICE BLUEPRINT
DIALOG: SUSTAINABLE BUSINESS MODEL CANVAS
FEEDBACK
“This project took our breath away. DiaLog looks at the problem of diagnosis limbo from multiple angles and provides a number of ways to track, understand, and connect around symptoms. The service is robust and offers a unique and fitting experience for every individual. We commend the team for using both qualitative and quantitative research to design a service with empathy at its core”
— Philips' Team
“DiaLog is a standout project in both societal relevance and design excellence. It successfully reframes diagnosis limbo as a condition worthy of recognition. DiaLog stands out as a model for responsible, inclusive service design in healthcare. It refines an eclectic experience. Delivers a credible and compassionate solution and demonstrates the systemic potential of design. When it centers human dignity. It bridges the gender health gap. Of women with measurable psychological and systemic benefits.”
— Eliisa Sarkkinen (Chapter Lead of the Service Design Network Finland)
“DiaLog will allow patients to feel satisfied in their approach to their illness and help build better interpersonal relationships, which invariably leads to better healthcare.”
— NHS Medical Doctor (MD)
“I would put all my notes and medical references into DiaLog if it existed. It simplifies things a lot.”
— Patient in 4-Year Diagnosis Limbo
IMPACT
Reduced repeat GP visits (projected 5–15%)
By improving narrative continuity and consultation readiness, fewer appointments are used to re-explain symptoms or restart diagnostic conversations.
More efficient consultations (projected time saved per visit)
Structured histories and clearer priorities support faster context-building and more focused clinical conversations within time-limited appointments.
Improved patient confidence and emotional wellbeing (projected 10–20% increased satisfaction)
Validation, continuity, and guided sense-making reduce anxiety and increase perceived agency during prolonged uncertainty.